Guidance to healthcare professionals on how to achieve the intended prescribed daily dose of Fostimon
What is Fostimon?
It is intended for subcutaneous or intramuscular administration1.
Fostimon 75 IU contains urofollitropin 75 IU, providing 75 IU of follicle stimulating hormone (FSH) activity.
Fostimon 150 IU contains urofollitropin 150 IU, providing 150 IU of FSH activity.
Fostimon is indicated for1:
- Anovulation (including polycystic ovarian syndrome) in women who have been unresponsive to treatment with clomifene citrate
- Controlled ovarian hyperstimulation to induce the development of multiple follicles in ART such as IVF, Gamete Intra-fallopian Transfer and Zygotes Intra-fallopian Transfer

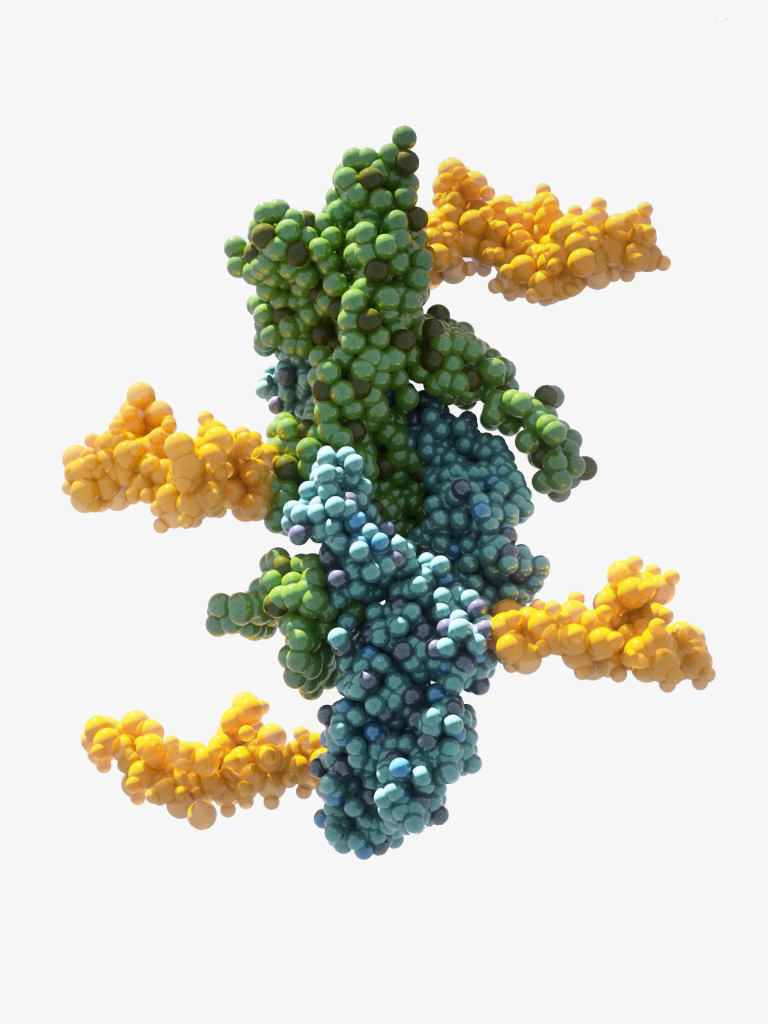
Acidic isoform profile.
Fostimon contains a mix of acidic FSH isoforms2, reflecting the early-to-mid follicular phase3-5. The level of glycosylation and sialyation of FSH molecules varies across the menstrual cycle. In the early-mid follicular phase, more acidic forms of FSH predominate and in the late follicular phase, approaching ovulation, less acidic forms of FSH predominate2.
Lombardi et al, used high pressure liquid chromatography/mass spectrometry and bioinformatics to identify the glycan content of human FSH preparations. The study demonstrated that Fostimon contains more acidic FSH isoforms than some recombinant FSH formulations2.
Efficacy.
A randomised, controlled, investigator-blinded trial in 152 IVF patients, aged 18-39 sought to compare the efficacy of highly purified human urinary follicle stimulating hormone (HP-hFSH, Fostimon) versus human recombinant follitropin-alpha (rFSH, Gonal-F) at a starting dose of 300IU in down-regulated cycles6.
Results
- The total IU of gonadotropin used did not differ between the two groups.
- There was no difference in number of oocytes retrieved with HP-hFSH (mean = 16.3) compared with rFSH (mean = 17.1), confidence interval (CI) of difference = -3.79 to +2.18.
- Clinical pregnancy rate, as defined by the presence of a gestational sac, was 48.7% (CI ¼ 37.0%-60.4%) with HP-hFSH versus 44.7% (CI ¼ 33.3%-56.6%) with rFSH (CI of difference ¼11.9% to þ19.8%).
- Live birth rate was 38.2% (29 of 76) in both groups (CI - 27.2%-50.0%), for a difference between groups of 0.0% (CI of the difference = -15.4% to +15.4%).
Conclusion(s): There were no statistically significant differences in mean oocyte number, clinical pregnancy rate, or live birth rate between HP-hFSH versus rFSH.
Efficacy.
Non-inferiority, prospective, controlled, randomised, multicentre studies have demonstrated that Fostimon is at least as effective and well tolerated as recombinant FSH7,8.
The first meta-analysis7 reported:
- No significant difference between Fostimon and recombinant FSH in ongoing pregnancy/live birth rate (OR 1.16; 95% Cl 0.91; 1.47)
- OHSS rate was not significantly different between the two treatments (OR 0.24; 95% Cl 0.03; 2.23)
The second meta-analysis8 showed no significant differences between:
- Recombinant FSH and Fostimon treatment in live birth rate (OR 0.84, 95% Cl 0.63; 1.11)
- Clinical pregnancy rate (OR 0.85, 95% Cl 0.68; 1.07)
- The number of oocytes retrieved, the number of mature oocytes, and days of stimulation

Safety information.
Contraindications
- Hypersensitivity to FSH or any of the excipients
- Tumours of the hypothalamus or pituitary gland and in females who have either ovarian enlargement or a cyst not due to polycystic ovarian disease
- Gynaecological bleeding of unknown origin
- Ovarian, uterine or mammary carcinoma
- Primary ovarian failure
- Malformations of sexual organs incompatible with pregnancy
- Fibroid tumours of the uterus incompatible with pregnancy
Adverse events
Some adverse reactions (ADRs) such as headache, abdominal distension and ovarian hyperstimulation syndrome were reported in clinical trials with Fostimon. Most events were of mild to moderate severity.
Refer to the SmPC for details on the full side effect profile, contraindications, warnings and interactions.
Additional resources.
-
Summary of Product Characteristics
Download

-
Prescribing Information
Download

-
Patient Resources
View

Additional studies.
- Smitz J, Wolfenson C, Chappel S, Ruman J. Follicle-Stimulating Hormone: A Review of Form and Function in the Treatment of Infertility. Reprod Sci. 2016;23(6):706-716. doi:10.1177/1933719115607992
- Conforti A, Esteves SC, Picarelli S, et al. Novel approaches for diagnosis and management of low prognosis patients in assisted reproductive technology: the POSEIDON concept. Panminerva Med. 2019;61(1):24-29. doi:10.23736/S0031-0808.18.03511-5
- Alviggi C, Pettersson K, Longobardi S, et al. A common polymorphic allele of the LH beta-subunit gene is associated with higher exogenous FSH consumption during controlled ovarian stimulation for assisted reproductive technology. Reprod Biol Endocrinol. 2013;11:51. Published 2013 Jun 1. doi:10.1186/1477-7827-11-51
References
- Fostimon Summary of Product Characteristics
- Lombardi A, Andreozzi C, Pavone V, Triglione V, Angiolini L, Caccia P. Evaluation of the oligosaccharide composition of commercial follicle stimulating hormone preparations. Electrophoresis. 2013;34(16):2394-2406. doi:10.1002/elps.201300045
- Vitt UA, Nayudu PL, Rose UM, Kloosterboer HJ. Embryonic Development after Follicle Culture Is Influenced by Follicle-Stimulating Hormone Isoelectric Point Range1. Biology of Reproduction. 2001;65(5):1542-1547. doi:https://doi.org/10.1095/biolreprod65.5.1542
- Andersen CY. Effect of FSH and its different isoforms on maturation of oocytes from pre-ovulatory follicles. Reproductive BioMedicine Online. 2002;5(3):232-239. doi:https://doi.org/10.1016/s1472-6483(10)61826-3
- Orvieto R, Venetis CA, Fatemi HM, et al. Optimising Follicular Development, Pituitary Suppression, Triggering and Luteal Phase Support During Assisted Reproductive Technology: A Delphi Consensus. Front Endocrinol (Lausanne). 2021;12:675670. Published 2021 May 10. doi:10.3389/fendo.2021.675670
- Baker VL, Fujimoto VY, Kettel LM, et al. Clinical efficacy of highly purified urinary FSH versus recombinant FSH in volunteers undergoing controlled ovarian stimulation for in vitro fertilization: a randomized, multicenter, investigator-blind trial. Fertility and Sterility. 2009;91(4):1005-1011. doi:https://doi.org/10.1016/j.fertnstert.2008.01.064
- Al-Inany HG, Abou-Setta AM. Are all human-derived follicle-stimulating hormone products the same? A systematic review and meta-analysis using direct and adjusted indirect analyses, to determine whether Fostimon®is more efficient than Metrodin-HP®. Gynecological Endocrinology. 2011;28(2):94-101. doi:https://doi.org/10.3109/09513590.2011.569612
- Gerli S, Bini V, Favilli A, Di Renzo GC. Clinical efficacy and cost-effectiveness of HP-human FSH (Fostimon®) versus rFSH (Gonal-F®) in IVF-ICSI cycles: a meta-analysis. Gynecological Endocrinology. 2013;29(6):520-529. doi:https://doi.org/10.3109/09513590.2012.758703
Adverse events should be reported. Reporting forms and information can be found at yellowcard.mhra.gov.uk.
Adverse events should also be reported to IBSA Pharma Ltd on 01923 233466 and medicalinformation.uk@ibsagroup.com.